The recent announcement of dedicated investment for Digital Asynchronous Consulting Systems (DACS) within the 2026 to 2029 GP contract presents a significant opportunity for Scottish Primary Care. This commitment offers more than just funding; it's a chance to move beyond incremental change and define a uniquely Scottish digital approach that is flexible, inclusive, and robust.
Since launching Accurx in Scotland in February 2025, growth has been rapid, from 3 pilot sites in Lothian to over 130 practices across the country. This adoption has highlighted that digital tools can be successfully delivered to both rural and urban settings, providing early insights into sustainable digital transformation in the Scottish landscape.
Five practical insights from scaling digital general practice across England to Scotland
1. Change does not need to be all or nothing
Accurx, which began as a simple SMS communication tool in 2016, evolved out of the essential, real-world needs of busy practices. Over time it expanded into structured messaging, questionnaires, video consultations, shared inboxes, self-booking links, and online triage. Accurx is now used by 96% of GPs in England.
Many practices choose to start their digital journey with Accurx with simple messaging or self-booking links, then add digital forms for admin requests before expanding to wider online triage model.
This steady approach builds staff and patient confidence, reduces disruption and allows teams to refine their model before scaling.
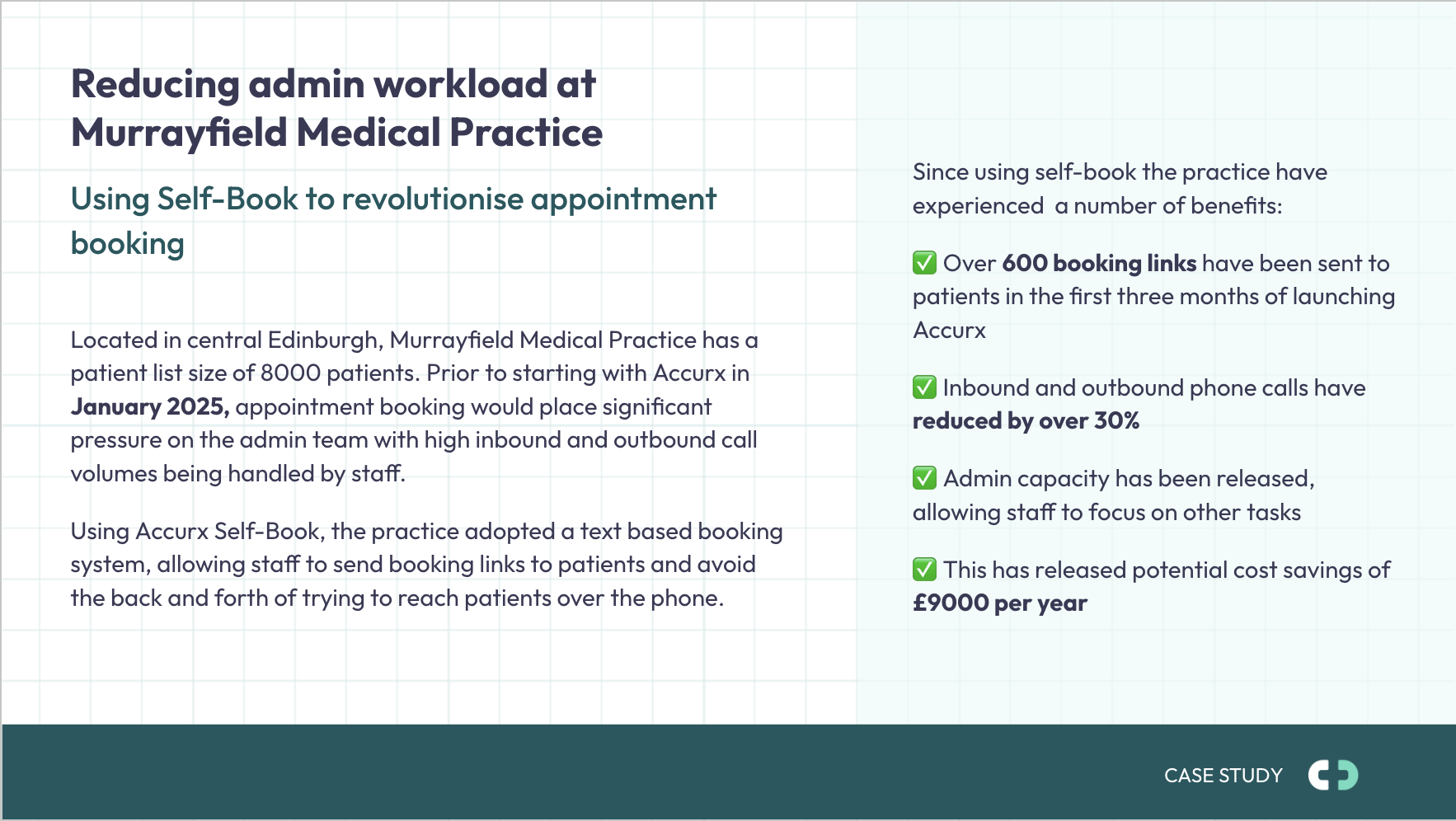
By introducing Accurx booking links and messaging alone, Murrayfield Medical Practice reduced inbound phone calls by over 30% in only three months.
2. Ruralilty or deprivation not barriers to digital adoption
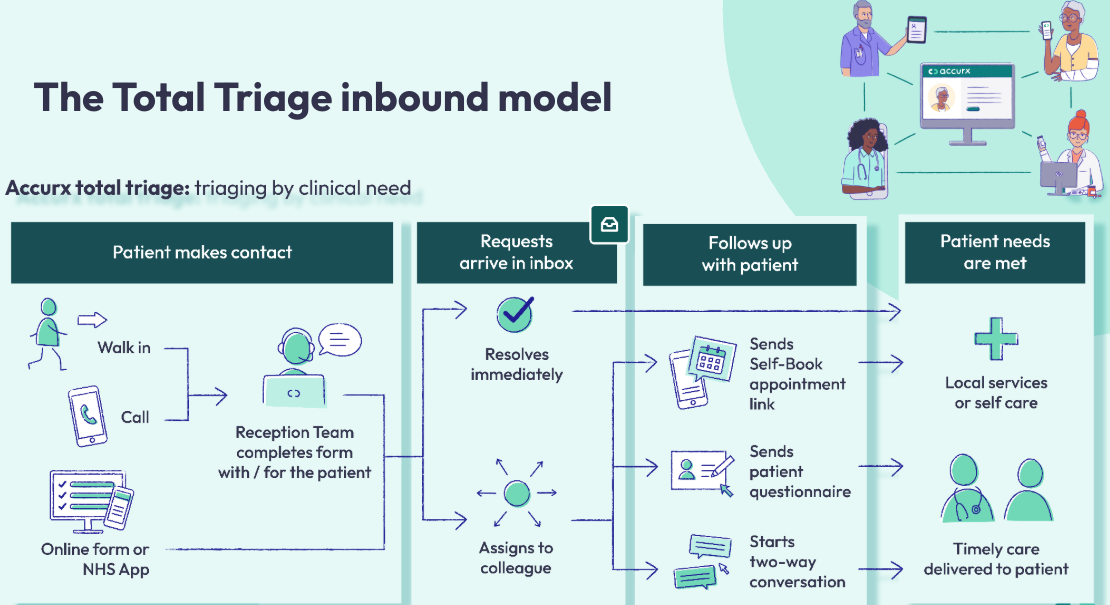
Total Triage is a model where all patient requests are managed in a single inbox and triaged to help manage demand and capacity. Some of the strongest outcomes in England have been seen in Total Triage practices serving the most deprived populations, and those in remote or semi-rural areas.
In Scotland, Skerryvore Medical Practice in Kirkwall, Orkney shows what is possible. Despite its remote location, digital pathways have helped stabilise workload and support small multidisciplinary teams, with 85 percent of surveyed patients saying the forms were very easy to use and the remaining 15 percent saying they were quite easy.
There is a widespread misconception that digital triage is less effective for older patients, people with low digital confidence, or those living in deprived communities. However, data from more than 1,350 practices using Accurx Total Triage across England directly challenges this assumption. Around one in ten of these practices are in the most deprived decile, and roughly a quarter are in the lowest two deciles for health, older people, or living environment deprivation.
Together, this shows that digital triage is being used successfully across a wide range of communities, including those facing the greatest levels of disadvantage.
It's important to note though that patients who cannot use the digital form are not excluded, as walk-ins and telephone routes often become more accessible for this group.
Many requests can also be better supported outside of general practice, and effective digital signposting can redirect around 20 to 40 percent of inbound demand to more appropriate services.
Taken together, the pattern is clear. Total triage is not confined to particular communities or practice types. For Scottish practices preparing for DACS, this should provide reassurance that digital access can be both inclusive and reliable across a wide range of patient groups.
3. Digital innovation supports the whole practice, not just GPs
The positive impact of digital tools can be seen across the primary care team; benefitting reception, nursing staff, and pharmacists.
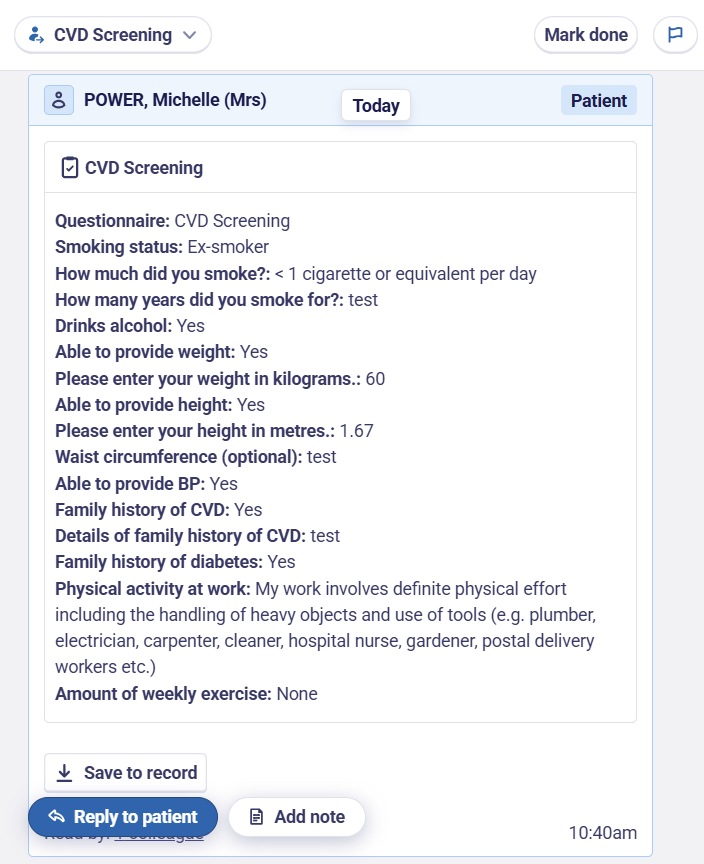
Reception report calmer mornings and quieter phone lines, with improved task management and a more predictable, structured workload. Nurses and pharmacists are using questionnaires to gather information asynchronously, allowing remote reviews and avoiding unnecessary appointments.
“We are finding the Accurx asthma templates really helpful. It is saving our admin team significant amounts of time speaking to patients on the phone and booking them in for asthma reviews. The practice nurses are able to focus their time on patients with poor control or who can step down preventer therapy. GPs can see the ACT scores coded in the notes, even for patients who do not have a face-to-face asthma review with a practice nurse." - Dr Anna Beedel, GP Partner at Prestonpans Group Practice, Edinburgh
4. Measure what matters
It’s helpful that practices consider which outcome data they will monitor to demonstrate the impact of digital transformation. When adopting new ways of working, measuring change will not only help to share the positive impact, but also to justify the investment.
Examples include:
- Monitoring Did Not Attend (DNA) rates following the introduction of self-booking links, as patients have more autonomy over their appointment times.
- Patient Triage dashboards to evaluate the conversion of requests closed without an appointment or signposted to more appropriate services.
- Cloud telephony data with online access, with less patients calling the practice.
Many total triage practices complete around 98% of requests within a day and report fewer missed calls, steadier demand and fewer peaks that overwhelm staff.
Cwmfelin Medical Practice saw a significant drop in inbound call volume from 7000 to 5000 calls per month from implementing total triage.
.png)
5. Learn from practices who have already done it
Peer learning is consistently highlighted as one of the key enablers of successful digital transformation.
Practices that introduced Total Triage in England report that visiting other sites, seeing workflows in action, and hearing directly from other primary care teams about their journey was invaluable.
As Scotland rolls out DACS and cloud telephony, the experience of early adopters can help other practices to design models that fit their own population and workforce, avoiding a fragmented system where neighbouring practices use completely different tools.
Looking beyond Scotland and learning from counterparts elsewhere will also help practices to avoid common pitfalls, accelerate implementation, and make more informed decisions based on real-world experience rather than theory alone.
Sign up to speak to a total triage ambassador here
Our takeaway
As the details from the new GP contract emerge, we are cautiously optimistic that it will provide the funding and infrastructure needed to modernise access sustainably. Lessons from Accurx’s scale in England demonstrate that digital tools work best when adopted gradually, shaped around local needs, and used across the whole practice team.
Starting with simple, impactful tools such as messaging or self-booking, before progressing to structured triage and shared workflows, offers a safe and effective path forward. With great intentions clearly set out Scotland now has the opportunity to modernise access in a way that reflects the realities of Scottish general practice, and the pressure its under.
